Hi northk,
Thanks for reaching out! I’m glad the message was heard. I’ve included some of the references below. It’s a long list, but hopefully you find a few that you’d like to read!
In terms of the fueling solution to balance health and performance, I don’t have a definitive answer for you on that. I’m still figuring it out myself. But as some guidelines:
- when performance is not key, favor foods that have carbohydrates but have a lower glycemic load. That generally means more natural foods where the sugars are bound
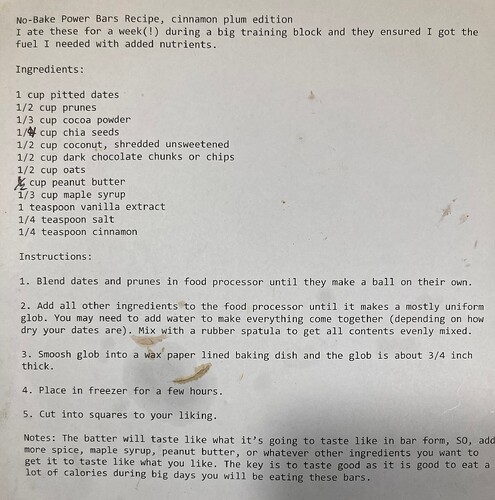
- making your own foods is great! I wish I had the time. If you can’t then I’d focus on getting bars that are again, more natural, and lower glycemic load. I’d favor those over gus and gels while just training.
- personally, I’ve been riding with beef jerky, but that’s not for everyone
I don’t know where the cut line is for too much sugar. I think that takes some personal exploration. I personally have a tell - when I eat too much, my AFIB acts up. And I can tell you that the line for me is very low. I can’t handle much. Hence my switch to beef jerky.
Hope that helps! Let me know what you find. In the meantime, here’s the references I promised you:
Adili, Ailiya, Xiyu Zhu, Hailong Cao, Xinlong Tang, Yali Wang, Junxia Wang, Jian Shi, Qing Zhou, and Dongjin Wang. 2022. “Atrial Fibrillation Underlies Cardiomyocyte Senescence and Contributes to Deleterious Atrial Remodeling during Disease Progression.” Aging and Disease 13 (1): 298–312. Atrial Fibrillation Underlies Cardiomyocyte Senescence and Contributes to Deleterious Atrial Remodeling during Disease Progression.
Aengevaeren, Vincent L., Arend Mosterd, Thijs L. Braber, Niek H.J. Prakken, Pieter A. Doevendans, Diederick E. Grobbee, Paul D. Thompson, Thijs M.H. Eijsvogels, and Birgitta K. Velthuis. 2017. “Relationship Between Lifelong Exercise Volume and Coronary Atherosclerosis in Athletes.” Circulation 136 (2): 138–48. https://doi.org/10.1161/circulationaha.117.027834.
Alpert, Joseph. 2021. “Recent Thoughts Concerning Atrial Fibrillation.” The American Journal of Medicine 135 (1): 1–2. Redirecting.
Ausland, Ådne, Edvard Liljedahl Sandberg, Jarle Jortveit, and Stephen Seiler. 2022. “Heart Rhythm Assessment in Elite Endurance Athletes: A Better Method?” Frontiers in Sports and Active Living 4:937525. Frontiers | Heart rhythm assessment in elite endurance athletes: A better method?.
Barrea, Luigi, Massimiliano Caprio, Dario Tuccinardi, Eleonora Moriconi, Laura Di Renzo, Giovanna Muscogiuri, Annamaria Colao, Silvia Savastano, and Education nutrition Research and Assessment (OPERA) group on behalf of the Obesity Programs of. 2022. “Could Ketogenic Diet ‘Starve’ Cancer? Emerging Evidence.” Critical Reviews in Food Science and Nutrition 62 (7): 1800–1821. https://doi.org/10.1080/10408398.2020.1847030.
Bartlett, Jonathan D., Graeme L. Close, Barry Drust, and James P. Morton. 2014. “The Emerging Role of P53 in Exercise Metabolism.” Sports Medicine 44 (3): 303–9. The Emerging Role of p53 in Exercise Metabolism | Sports Medicine.
Bernat-Adell, María D, Eladio J Collado-Boira, Pilar Moles-Julio, Nayara Panizo-González, Ignacio Martínez-Navarro, Bárbara Hernando-Fuster, and Carlos Hernando-Domingo. 2021. “Recovery of Inflammation, Cardiac, and Muscle Damage Biomarkers After Running a Marathon.” Journal of Strength and Conditioning Research 35 (3): 626–32. The Journal of Strength & Conditioning Research.
Buckley, Benjamin J. R., Gregory Y. H. Lip, and Dick H. J. Thijssen. 2020. “The Counterintuitive Role of Exercise in the Prevention and Cause of Atrial Fibrillation.” American Journal of Physiology-Heart and Circulatory Physiology 319 (5): H1051–58. https://doi.org/10.1152/ajpheart.00509.2020.
Calvo, Naiara, Josep Brugada, Marta Sitges, and Lluís Mont. 2012. “Atrial Fibrillation and Atrial Flutter in Athletes.” British Journal of Sports Medicine 46 (Suppl 1): i37. https://doi.org/10.1136/bjsports-2012-091171.
Canbolat, Eren, and Funda Pınar Cakıroglu. 2023. “The Importance of AMPK in Obesity and Chronic Diseases and the Relationship of AMPK with Nutrition: A Literature Review.” Critical Reviews in Food Science and Nutrition 63 (4): 449–56. https://doi.org/10.1080/10408398.2022.2087595.
Carling, David. 2017. “AMPK Signalling in Health and Disease.” Current Opinion in Cell Biology 45:31–37. Redirecting.
Chen, Yi Ching, Aleksandr Voskoboinik, Andre La Gerche, Thomas H. Marwick, and Julie R. McMullen. 2021. “Prevention of Pathological Atrial Remodeling and Atrial Fibrillation JACC State-of-the-Art Review.” Journal of the American College of Cardiology 77 (22): 2846–64. Redirecting.
Chrienova, Zofia, Eugenie Nepovimova, and Kamil Kuca. 2021. “The Role of MTOR in Age-Related Diseases.” Journal of Enzyme Inhibition and Medicinal Chemistry 36 (1): 1678–92. https://doi.org/10.1080/14756366.2021.1955873.
Dazert, Eva, and Michael N Hall. 2011. “MTOR Signaling in Disease.” Current Opinion in Cell Biology 23 (6): 744–55. Redirecting.
Draznin, B, C Wang, R Adochio, J Leitner, and M -A Cornier. 2012. “Effect of Dietary Macronutrient Composition on AMPK and SIRT1 Expression and Activity in Human Skeletal Muscle.” Hormone and Metabolic Research 44 (09): 650–55. Thieme E-Journals - Hormone and Metabolic Research / Abstract.
Dyńka, Damian, Katarzyna Kowalcze, and Agnieszka Paziewska. 2022. “The Role of Ketogenic Diet in the Treatment of Neurological Diseases.” Nutrients 14 (23): 5003. Nutrients | Free Full-Text | The Role of Ketogenic Diet in the Treatment of Neurological Diseases.
Elliott, Adrian D., Christian V. Verdicchio, Celine Gallagher, Dominik Linz, Rajiv Mahajan, Ricardo Mishima, Kadhim Kadhim, et al. 2021. “Factors Contributing to Exercise Intolerance in Patients With Atrial Fibrillation.” Heart, Lung and Circulation 30 (7): 947–54. Redirecting.
Fell, J. Marc, Mark A. Hearris, Daniel G. Ellis, James E. P. Moran, Emily F. P. Jevons, Daniel J. Owens, Juliette A. Strauss, et al. 2021. “Carbohydrate Improves Exercise Capacity but Does Not Affect Subcellular Lipid Droplet Morphology, AMPK and P53 Signalling in Human Skeletal Muscle.” The Journal of Physiology 599 (11): 2823–49. https://doi.org/10.1113/jp281127.
Fontana, Luigi, Timothy E. Meyer, Samuel Klein, and John O. Holloszy. 2004. “Long-Term Calorie Restriction Is Highly Effective in Reducing the Risk for Atherosclerosis in Humans.” Proceedings of the National Academy of Sciences 101 (17): 6659–63. https://doi.org/10.1073/pnas.0308291101.
Fontana, Luigi, Linda Partridge, and Valter D. Longo. 2010. “Extending Healthy Life Span—From Yeast to Humans.” Science 328 (5976): 321–26. https://doi.org/10.1126/science.1172539.
Garza, Maria Sanz-de la, Cira Rubies, Montserrat Batlle, Bart H. Bijnens, Lluis Mont, Marta Sitges, and Eduard Guasch. 2017. “Severity of Structural and Functional Right Ventricular Remodeling Depends on Training Load in an Experimental Model of Endurance Exercise.” American Journal of Physiology-Heart and Circulatory Physiology 313 (3): H459–68. https://doi.org/10.1152/ajpheart.00763.2016.
Ge, Yuchen, Min Zhou, Cui Chen, Xiaojian Wu, and Xiaobo Wang. 2022. “Role of AMPK Mediated Pathways in Autophagy and Aging.” Biochimie 195:100–113. Redirecting.
Gerche, André La, Aaron Baggish, Hein Heidbuchel, Benjamin D. Levine, and Dhrubo Rakhit. 2018. “What May the Future Hold for Sports Cardiology?” Heart, Lung and Circulation 27 (9): 1116–20. Redirecting.
Guo, Jun, Xiuqing Huang, Lin Dou, Mingjing Yan, Tao Shen, Weiqing Tang, and Jian Li. 2022. “Aging and Aging-Related Diseases: From Molecular Mechanisms to Interventions and Treatments.” Signal Transduction and Targeted Therapy 7 (1): 391. Aging and aging-related diseases: from molecular mechanisms to interventions and treatments | Signal Transduction and Targeted Therapy.
Gurukripa, N. Kowlgi, M. Agboola Kolade, and G. Allison Thomas. 2021. “Atrial Fibrillation in the Athlete: Case Report and a Contemporary Appraisal.” Journal of Electrocardiology 66:6–11. Redirecting.
Harada, Masahide, Sarah Naomi Nattel, and Stanley Nattel. 2018. “AMP-Activated Protein Kinase.” Circulation: Arrhythmia and Electrophysiology 5 (4): 860–67. https://doi.org/10.1161/circep.112.972265.
Harada, Masahide, Artavazd Tadevosyan, Xiaoyan Qi, Jiening Xiao, Tao Liu, Niels Voigt, Matthias Karck, et al. 2015. “Atrial Fibrillation Activates AMP-Dependent Protein Kinase and Its Regulation of Cellular Calcium Handling Potential Role in Metabolic Adaptation and Prevention of Progression.” Journal of the American College of Cardiology 66 (1): 47–58. Redirecting.
Heidbuchel, Hein, Michael Papadakis, Nicole Panhuyzen-Goedkoop, François Carré, Dorian Dugmore, Klaus-Peter Mellwig, Hanne Kruuse Rasmusen, et al. 2012. “Position Paper: Proposal for a Core Curriculum for a European Sports Cardiology Qualification.” European Journal of Preventive Cardiology 20 (5): 889–903. Position paper: proposal for a core curriculum for a European Sports Cardiology qualification | European Journal of Preventive Cardiology | Oxford Academic.
“Identification of a Leucine-Mediated Threshold Effect Governing Macrophage MTOR Signalling and Cardiovascular Risk.” n.d. Identification of a leucine-mediated threshold effect governing macrophage mTOR signalling and cardiovascular risk | Nature Metabolism.
Javed, Wasim, Nathan J Price, Christopher ED Saunderson, Adam K McDiarmid, Bara Erhayiem, Maryum Farooq, James O’Neill, et al. 2022. “Cardiovascular Magnetic Resonance Assessment of Left Atrial Size and Function in Endurance Athletes.” Future Cardiology 18 (9): 697–707. https://doi.org/10.2217/fca-2021-0151.
Jesel, Laurence, Malak Abbas, Sin-Hee Park, Kensuke Matsushita, Michel Kindo, Hira Hasan, Cyril Auger, et al. 2019. “Atrial Fibrillation Progression Is Associated with Cell Senescence Burden as Determined by P53 and P16 Expression.” Journal of Clinical Medicine 9 (1): 36. JCM | Free Full-Text | Atrial Fibrillation Progression Is Associated with Cell Senescence Burden as Determined by p53 and p16 Expression.
K, Mohit, Turagam Md, Greg C, Flaker Md, Poonam Velagapudi Md, Sirisha Vadali Md, Martin A, and Alpert Md. 2015. “Atrial Fibrillation In Athletes: Pathophysiology, Clinical Presentation, Evaluation and Management.” Journal of Atrial Fibrillation 8 (4): 1309. https://doi.org/10.4022/jafib.1309.
Katsuumi, Goro, Ippei Shimizu, Yohko Yoshida, and Tohru Minamino. 2018. “Vascular Senescence in Cardiovascular and Metabolic Diseases.” Frontiers in Cardiovascular Medicine 5:18. Frontiers | Vascular Senescence in Cardiovascular and Metabolic Diseases.
Khan, Ali K, Hyon Jae Lee, Mellanie T Hills, Melissa Moss, Brenna Lara, Raymond Baumann, Cynthia Brandt, and Rachel J Lampert. 2022. “Abstract 10548: Atrial Fibrillation Worsens Sports Performance in Athletes; Greatest Improvement Seen With Ablation: A Stopafib.Org Survey.” Circulation 146 (Suppl_1): A10548–A10548. https://doi.org/10.1161/circ.146.suppl_1.10548.
Kim, Joungmok, Goowon Yang, Yeji Kim, Jin Kim, and Joohun Ha. 2016. “AMPK Activators: Mechanisms of Action and Physiological Activities.” Experimental & Molecular Medicine 48 (4): e224–e224. AMPK activators: mechanisms of action and physiological activities | Experimental & Molecular Medicine.
KO, JOUNGBO, YOUNG C. JANG, JOHN QUINDRY, RODNEY GUTTMANN, LUDMILA COSIO-LIMA, SCOTT K. POWERS, and YOUNGIL LEE. 2023. “Exercise-Induced Antisenescence and Autophagy Restoration Mitigate Metabolic Disorder–Induced Cardiac Disruption in Mice.” Medicine & Science in Sports & Exercise 55 (3): 376–88. Medicine & Science in Sports & Exercise.
LaGerche, André, Siddharth J Trivedi, Guido Claessen, and Liza Thomas. 2021. “Response to Sanchis-Gomar et al. ‘Atrial Fibrillation in Athletes and Non-Athletes: Evidence of Different Causative Mechanisms.’” European Heart Journal - Cardiovascular Imaging 22 (6): 722–722. Response to Sanchis-Gomar et al. ‘Atrial fibrillation in athletes and non-athletes: evidence of different causative mechanisms’ | European Heart Journal - Cardiovascular Imaging | Oxford Academic.
Laplante, Mathieu, and David M. Sabatini. 2012. “MTOR Signaling in Growth Control and Disease.” Cell 149 (2): 274–93. Redirecting.
Liu, Yaozhong, Fan Bai, Na Liu, Feifan Ouyang, and Qiming Liu. 2019. “The Warburg Effect: A New Insight into Atrial Fibrillation.” Clinica Chimica Acta 499:4–12. Redirecting.
Lyons, Claire L., and Helen M. Roche. 2018. “Nutritional Modulation of AMPK-Impact upon Metabolic-Inflammation.” International Journal of Molecular Sciences 19 (10): 3092. IJMS | Free Full-Text | Nutritional Modulation of AMPK-Impact upon Metabolic-Inflammation.
Madan, Esha, Rajan Gogna, Madan Bhatt, Uttam Pati, Periannan Kuppusamy, and Abbas Ali Mahdi. 2011. “Regulation of Glucose Metabolism by P53: Emerging New Roles for the Tumor Suppressor.” Oncotarget 2 (12): 948–57. Regulation of glucose metabolism by p53: Emerging new roles for the tumor suppressor | Oncotarget.
Mahjoub, Haïfa, Olivier Le Blanc, Myriam Paquette, Sarah Imhoff, Lawrence Labrecque, Audrey Drapeau, Paul Poirier, Élisabeth Bédard, Philippe Pibarot, and Patrice Brassard. 2019. “Cardiac Remodeling after Six Weeks of High-Intensity Interval Training to Exhaustion in Endurance-Trained Men.” American Journal of Physiology. Heart and Circulatory Physiology 317 (4): H685–94. https://doi.org/10.1152/ajpheart.00196.2019.
Miguel-dos-Santos, Rodrigo, José Bianco Nascimento Moreira, Jan Pål Loennechen, Ulrik Wisløff, and Thássio Mesquita. 2021. “Exercising Immune Cells: The Immunomodulatory Role of Exercise on Atrial Fibrillation.” Progress in Cardiovascular Diseases 68:52–59. Redirecting.
Mohammed, Ibrahim, Morley D. Hollenberg, Hong Ding, and Chris R. Triggle. 2021. “A Critical Review of the Evidence That Metformin Is a Putative Anti-Aging Drug That Enhances Healthspan and Extends Lifespan.” Frontiers in Endocrinology 12:718942. Frontiers | A Critical Review of the Evidence That Metformin Is a Putative Anti-Aging Drug That Enhances Healthspan and Extends Lifespan.
Newman, William, Gemma Parry-Williams, Jonathan Wiles, Jamie Edwards, Sabina Hulbert, Konstantina Kipourou, Michael Papadakis, Rajan Sharma, and Jamie O’Driscoll. 2021. “Risk of Atrial Fibrillation in Athletes: A Systematic Review and Meta-Analysis.” British Journal of Sports Medicine 55 (21): 1233–38. https://doi.org/10.1136/bjsports-2021-103994.
Oh, Yena, Sibao Yang, Xueyan Liu, Sayantan Jana, Farzad Izaddoustdar, Xiaodong Gao, Ryan Debi, et al. 2020. “Transcriptomic Bioinformatic Analyses of Atria Uncover Involvement of Pathways Related to Strain and Post-Translational Modification of Collagen in Increased Atrial Fibrillation Vulnerability in Intensely Exercised Mice.” Frontiers in Physiology 11:605671. Frontiers | Transcriptomic Bioinformatic Analyses of Atria Uncover Involvement of Pathways Related to Strain and Post-translational Modification of Collagen in Increased Atrial Fibrillation Vulnerability in Intensely Exercised Mice.
Ozcan, Cevher, Gunjan Dixit, and Zhenping Li. 2021. “Activation of AMP-Activated Protein Kinases Prevents Atrial Fibrillation.” Journal of Cardiovascular Translational Research 14 (3): 492–502. Activation of AMP-Activated Protein Kinases Prevents Atrial Fibrillation | Journal of Cardiovascular Translational Research.
Papaconstantinou, John. 2019. “The Role of Signaling Pathways of Inflammation and Oxidative Stress in Development of Senescence and Aging Phenotypes in Cardiovascular Disease.” Cells 8 (11): 1383. Cells | Free Full-Text | The Role of Signaling Pathways of Inflammation and Oxidative Stress in Development of Senescence and Aging Phenotypes in Cardiovascular Disease.
Papadopoli, David, Karine Boulay, Lawrence Kazak, Michael Pollak, Frédérick A. Mallette, Ivan Topisirovic, and Laura Hulea. 2019. “MTOR as a Central Regulator of Lifespan and Aging.” F1000Research 8:F1000 Faculty Rev-998. https://doi.org/10.12688/f1000research.17196.1.
Pascale, Rosa Maria, Diego Francesco Calvisi, Maria Maddalena Simile, Claudio Francesco Feo, and Francesco Feo. 2020. “The Warburg Effect 97 Years after Its Discovery.” Cancers 12 (10): 2819. Cancers | Free Full-Text | The Warburg Effect 97 Years after Its Discovery.
Pieczenik, Steve R., and John Neustadt. 2007. “Mitochondrial Dysfunction and Molecular Pathways of Disease.” Experimental and Molecular Pathology 83 (1): 84–92. https://doi.org/10.1016/j.yexmp.2006.09.008.
Pokhrel, Ram Hari, Ben Kang, Maheshwor Timilshina, and Jae-Hoon Chang. 2022. “AMPK Amplifies IL2–STAT5 Signaling to Maintain Stability of Regulatory T Cells in Aged Mice.” International Journal of Molecular Sciences 23 (20): 12384. https://doi.org/10.3390/ijms232012384.
Rubinsztein, David C., Guillermo Mariño, and Guido Kroemer. 2011. “Autophagy and Aging.” Cell 146 (5): 682–95. https://doi.org/10.1016/j.cell.2011.07.030.
Sanchis-Gomar, Fabian, Fernando de la Guía-Galipienso, and Carl J Lavie. 2021. “Atrial Fibrillation in Athletes and Non-Athletes: Evidence of Different Causative Mechanisms.” European Heart Journal - Cardiovascular Imaging 22 (6): 723–723. https://doi.org/10.1093/ehjci/jeab018.
San-Millán, Iñigo, and George A. Brooks. 2017. “Reexamining Cancer Metabolism: Lactate Production for Carcinogenesis Could Be the Purpose and Explanation of the Warburg Effect.” Carcinogenesis, Carcinogenesis, 38 (2): 119–33. https://doi.org/10.1093/carcin/bgw127.
Saxton, Robert A., and David M. Sabatini. 2017. “MTOR Signaling in Growth, Metabolism, and Disease.” Cell 168 (6): 960–76. https://doi.org/10.1016/j.cell.2017.02.004.
Schmidt, Valentina, Rachana Nagar, and Luis A. Martinez. 2017. “Control of Nucleotide Metabolism Enables Mutant P53’s Oncogenic Gain-of-Function Activity.” International Journal of Molecular Sciences 18 (12): 2759. https://doi.org/10.3390/ijms18122759.
Sergeeva, Ekaterina, Tatiana Ruksha, and Yulia Fefelova. 2023. “Effects of Obesity and Calorie Restriction on Cancer Development.” International Journal of Molecular Sciences 24 (11): 9601. https://doi.org/10.3390/ijms24119601.
Shrier, Ian. 2015. “Strategic Assessment of Risk and Risk Tolerance (StARRT) Framework for Return-to-Play Decision-Making.” British Journal of Sports Medicine 49 (20): 1311. https://doi.org/10.1136/bjsports-2014-094569.
Stubbs, Marion, Paul M.J McSheehy, John R Griffiths, and C.Lindsay Bashford. 2000. “Causes and Consequences of Tumour Acidity and Implications for Treatment.” Molecular Medicine Today 6 (1): 15–19. https://doi.org/10.1016/s1357-4310(99)01615-9.
Su, Kevin N., Yina Ma, Marine Cacheux, Zeki Ilkan, Nour Raad, Grace K. Muller, Xiaohong Wu, et al. 2022. “Atrial AMP-Activated Protein Kinase Is Critical for Prevention of Dysregulation of Electrical Excitability and Atrial Fibrillation.” JCI Insight 7 (8): e141213. https://doi.org/10.1172/jci.insight.141213.
Tachtsis, Bill, William J. Smiles, Steven C. Lane, John A. Hawley, and Donny M. Camera. 2016. “Acute Endurance Exercise Induces Nuclear P53 Abundance in Human Skeletal Muscle.” Frontiers in Physiology 7:144. https://doi.org/10.3389/fphys.2016.00144.
Tran, Quangdon, Hyunji Lee, Chaeyeong Kim, Gyeyeong Kong, Nayoung Gong, So Hee Kwon, Jisoo Park, Seon-Hwan Kim, and Jongsun Park. 2020. “Revisiting the Warburg Effect: Diet-Based Strategies for Cancer Prevention.” BioMed Research International 2020:8105735. https://doi.org/10.1155/2020/8105735.
Trivedi, Siddharth J, Guido Claessen, Luke Stefani, M Darragh Flannery, Paula Brown, Kristel Janssens, Adrian Elliott, et al. 2020. “Differing Mechanisms of Atrial Fibrillation in Athletes and Non-Athletes: Alterations in Atrial Structure and Function.” European Heart Journal - Cardiovascular Imaging 21 (12): 1374–83. https://doi.org/10.1093/ehjci/jeaa183.
Valenzuela, Pedro L, Javier S Morales, Alejandro Santos-Lozano, Gonzalo Saco-Ledo, Leonel Diaz-Gonzalez, Araceli Boraita, Carl J Lavie, and Alejandro Lucia. 2021. “What Do We Really Know about the Association between Physical Activity, Sports, and Atrial Fibrillation? A Systematic Review and Meta-Analysis from Unbiased Studies.” European Journal of Preventive Cardiology. https://doi.org/10.1093/eurjpc/zwab073.
Wang, Zhiyu, Neng Wang, Pengxi Liu, and Xiaoming Xie. 2016. “AMP-Activated Protein Kinase.” Experientia Supplementum 107:203–26. https://doi.org/10.1007/978-3-319-43589-3_9.
Weiner, Rory B., and Aaron L. Baggish. 2012. “Exercise-Induced Cardiac Remodeling.” Progress in Cardiovascular Diseases 54 (5): 380–86. https://doi.org/10.1016/j.pcad.2012.01.006.
Xia, Yuxuan, Li Zhang, Dickson Kofi Wiredu Ocansey, Qiang Tu, Fei Mao, and Xiumei Sheng. 2023. “Role of Glycolysis in Inflammatory Bowel Disease and Its Associated Colorectal Cancer.” Frontiers in Endocrinology 14:1242991. https://doi.org/10.3389/fendo.2023.1242991.
Xu, Sha, Hui Tao, Wei Cao, Li Cao, Yan Lin, Shi-Min Zhao, Wei Xu, Jing Cao, and Jian-Yuan Zhao. 2021. “Ketogenic Diets Inhibit Mitochondrial Biogenesis and Induce Cardiac Fibrosis.” Signal Transduction and Targeted Therapy 6 (1): 54. https://doi.org/10.1038/s41392-020-00411-4.
Yavari, Arash, Mohamed Bellahcene, Annalisa Bucchi, Syevda Sirenko, Katalin Pinter, Neil Herring, Julia J. Jung, et al. 2017. “Mammalian Γ2 AMPK Regulates Intrinsic Heart Rate.” Nature Communications 8 (1): 1258. https://doi.org/10.1038/s41467-017-01342-5.
Yu, Miao, Brenee King, Emily Ewert, Xiaoyu Su, Nur Mardiyati, Zhihui Zhao, and Weiqun Wang. 2016. “Exercise Activates P53 and Negatively Regulates IGF-1 Pathway in Epidermis within a Skin Cancer Model.” PLoS ONE 11 (8): e0160939. https://doi.org/10.1371/journal.pone.0160939.
Zhou, Yifan, and Feng Liu. 2022. “Coordination of the AMPK, Akt, MTOR, and P53 Pathways under Glucose Starvation.” International Journal of Molecular Sciences 23 (23): 14945. https://doi.org/10.3390/ijms232314945.